Provider Credentialing
Ensure Compliance and Streamline Your Operations with Expert Provider Credentialing Services!

Provider Credentialing
At Health Care Protectors, we offer specialized Provider Credentialing services designed to simplify the credentialing process and ensure compliance with payer and regulatory requirements for healthcare providers. Our team is dedicated to managing and maintaining accurate credentialing records, allowing you to focus on providing exceptional patient care.
Why Provider Credentialing Matters
Provider credentialing is a critical component of a successful healthcare practice. Proper credentialing ensures that healthcare providers are qualified, meet industry standards, and are authorized to provide care. Here’s why you should consider our Provider Credentialing services:
- Compliance: Ensure compliance with payer and regulatory requirements to avoid penalties and fines.
- Accurate Records: Maintain accurate and up-to-date credentialing records for all providers.
- Streamlined Processes: Simplify the credentialing process to save time and resources.
- Revenue Optimization: Maximize reimbursements by ensuring providers are credentialed with all necessary payers.
Our Approach
At Health Care Protectors, we adopt a meticulous and client-focused approach to provider credentialing:
Credentialing Application Management:
- Application Preparation: We prepare and submit credentialing applications for healthcare providers, ensuring that all required documentation is complete and accurate. This includes gathering necessary information such as education, training, licensure, certifications, and work history.
- Submission and Follow-Up: We submit credentialing applications to payers and follow up to ensure timely processing. Our team tracks the status of each application and communicates with payers to resolve any issues that may arise.
- Re-Credentialing: We manage the re-credentialing process for providers, ensuring that their credentials are kept current and compliant with payer requirements.
Primary Source Verification:
- Verification Process: We conduct primary source verification of providers’ credentials, including education, training, licensure, and certifications. This ensures that all information provided is accurate and meets industry standards.
- Compliance with Standards: Our verification process complies with industry standards, including those set by the National Committee for Quality Assurance (NCQA) and the Joint Commission.
Ongoing Monitoring and Updates:
- Continuous Monitoring: We continuously monitor providers’ credentials to ensure they remain in compliance with payer and regulatory requirements. This includes tracking expiration dates for licenses and certifications and ensuring timely renewals.
- Regular Updates: We update credentialing records regularly to reflect any changes in providers’ qualifications, such as new certifications or changes in licensure status.
Network Enrollment:
- Payer Enrollment: We manage the enrollment of providers with insurance payers, ensuring that they are credentialed with all necessary payers to maximize reimbursements. This includes Medicare, Medicaid, and commercial insurance plans.
- Contract Management: We handle contract negotiations and management with payers, ensuring that providers are enrolled under favorable terms and conditions.
Compliance Assurance:
- Regulatory Compliance: We ensure that all credentialing practices comply with regulatory requirements and payer guidelines. This minimizes the risk of penalties and fines associated with non-compliance.
- Documentation and Record-Keeping: We maintain accurate and complete documentation of all credentialing activities, ensuring that records are readily available for audits and inspections.
Reporting and Analytics:
- Detailed Reporting: We provide detailed reports on credentialing activities, including the status of applications, verification results, and compliance metrics. These reports offer valuable insights into the credentialing process and help identify areas for improvement.
- Analytics Tools: Utilize advanced analytics tools to track key performance indicators (KPIs) and identify trends in credentialing activities. This data-driven approach helps optimize the credentialing process and enhance compliance.

AR Follow Up
Take control of your financial future with our specialized accounting services – Click here for details.
Audit Support
Let us handle the numbers, so you can focus on growth – Contact us now for accounting services.
Social Media Marketing
Elevate Your Brand's Voice – Social Media Marketing That Connects, Engages, and Grows!
Website Development
Transform Your Vision into Reality – Stunning, Functional Websites Built for Success!
Benefits of Outsourcing Credentialing
- Time Savings: Outsourcing can save significant time for your internal staff, allowing them to focus on patient care and other revenue-generating activities.
- Expertise: Credentialing companies have specialized knowledge and experience in navigating payer requirements and regulatory standards.
- Compliance: Ensures compliance with industry standards and reduces the risk of penalties and fines.
Statistics and Impact
Studies show that effective provider credentialing can lead to a 10-20% increase in reimbursements for healthcare practices. Additionally, practices that maintain accurate and up-to-date credentialing records see a 30% reduction in claim denials related to provider credentialing issues. These improvements not only boost your financial health but also enhance the efficiency and compliance of your practice.
Effective credentialing also contributes to patient trust and safety. By ensuring that all providers are qualified and meet industry standards, you can deliver higher quality care and build confidence among your patients.
Our comprehensive approach to provider credentialing ensures that every aspect of the credentialing process is handled with precision and care. From preparing and submitting applications to managing ongoing compliance, we cover all bases to ensure that your providers are credentialed and authorized to provide care.
Meet Our Doctors
Dr. Faika Khan
Dr. John Muney
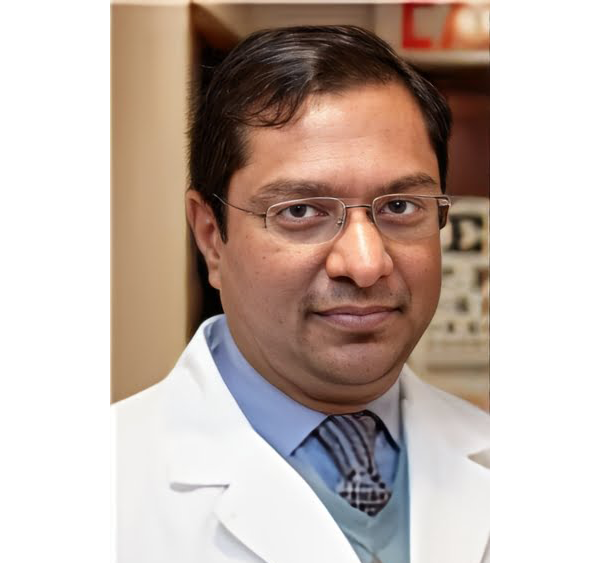
Dr. Ravindra Kashyap
Dr. Valerie Brutus
Your questions answered
Frequently Asked Questions (FAQs)
What is Provider Credentialing?
Provider Credentialing is the process of verifying and validating the qualifications, licensure, and certifications of healthcare providers. It ensures that providers meet industry standards and are authorized to provide care.
Why is credentialing important for healthcare providers?
Credentialing ensures that healthcare providers are qualified and meet regulatory requirements. It is essential for maintaining compliance, maximizing reimbursements, and building patient trust.
How do you manage the credentialing application process?
We prepare and submit credentialing applications, ensuring that all required documentation is complete and accurate. We follow up with payers to ensure timely processing and manage the re-credentialing process to keep providers’ credentials current.
What is primary source verification?
Primary source verification involves verifying providers’ credentials directly from the original source, such as educational institutions, licensing boards, and certification bodies. This ensures the accuracy and validity of the information provided.
How do you ensure compliance with regulatory requirements?
We stay updated with regulatory requirements and payer guidelines. Our credentialing practices comply with industry standards, including those set by NCQA and the Joint Commission. We maintain accurate documentation and regularly monitor providers’ credentials.
How do your services help reduce claim denials related to credentialing issues?
By ensuring that providers are credentialed with all necessary payers and maintaining accurate credentialing records, we minimize the risk of claim denials related to credentialing issues. Our proactive approach ensures that providers’ credentials are always current and compliant.
How do you handle network enrollment with insurance payers?
We manage the enrollment of providers with insurance payers, including Medicare, Medicaid, and commercial insurance plans. We handle contract negotiations and management to ensure favorable terms and conditions for providers.
How do we get started with Health Care Protectors' Provider Credentialing services?
Getting started is simple. Just contact us through our website or give us a call. Our team will guide you through the process and customize a credentialing plan that meets your practice’s needs.
Ready to ensure compliance and streamline your operations? Contact Health Care Protectors today to learn more about our expert Provider Credentialing services and how we can help your practice thrive