Medical Billing
Optimize Your Revenue Cycle with Expert Medical Billing Services!

Medical Billing
At Health Care Protectors, we offer specialized Medical Billing services designed to streamline your billing processes and maximize revenue for medical practices, including urgent care, primary care, specialty clinics, and more. Our team is dedicated to ensuring accurate charge creation, efficient billing, and effective management of problem lists, allowing you to focus on providing exceptional patient care.
Why Medical Billing Matters
Efficient medical billing is a critical component of a successful practice. Proper billing processes help reduce claim denials, ensure timely reimbursements, and optimize revenue. Here is why you should consider our Medical Billing services:
- Accurate Charge Entry: Ensure precise charge creation and entry to minimize errors and optimize revenue.
- Timely Billing: Expedite the billing process to reduce payment delays and improve cash flow.
- Compliance: Ensure compliance with payer guidelines and regulatory standards to avoid penalties and fines.
- Problem List Management: Maintain accurate and up-to-date problem lists to ensure comprehensive patient care and accurate coding.
Revenue Optimization: Maximize reimbursements and revenue through efficient and accurate billing practices.
Our Approach
At Health Care Protectors, we adopt a meticulous and client-focused approach to medical billing:
Accurate Charge Creation: Our process starts with the careful and precise creation of charges based on the medical services provided. This involves a detailed review of all medical documentation and the use of advanced coding systems to ensure that the charges entered are accurate. Accurate charge creation minimizes billing errors that can lead to claim denials and delays in payment. We collaborate closely with your medical staff to understand the services rendered and ensure that every charge is correctly documented.
Timely Billing Submission: The speed at which claims are submitted can significantly impact cash flow. We utilize advanced billing software to expedite the submission process. By submitting claims promptly, we reduce payment delays, allowing your practice to maintain a steady cash flow and avoid financial strain. Timely submission also ensures that claims are processed within the payer’s filing deadlines, preventing denials due to late submissions.
Compliance Assurance: Keeping up with payer guidelines and regulatory standards is essential for avoiding penalties and fines. Our team stays updated with the latest changes in regulations and payer policies. We ensure that all billing practices comply with these standards, minimizing the risk of non-compliance. This includes adhering to HIPAA regulations to protect patient information and following guidelines for accurate coding and billing.
Detailed Reporting: Transparency and insight are key to effective financial management. We provide detailed billing reports that include information on submitted claims, payment statuses, denial rates, and more. These reports offer a comprehensive view of your practice’s financial health, helping you make informed decisions. The reports also highlight areas where improvements can be made, enabling you to optimize your billing processes further.
Problem List Management: Accurate problem lists are vital for effective patient management and billing. We maintain and update problem lists, ensuring that all diagnoses are accurately documented and coded. This process ensures comprehensive patient care and supports precise billing. By keeping problem lists current, we help prevent missed diagnoses and ensure that all relevant conditions are considered during patient care.
Patient Insurance Verification: Verifying patient insurance coverage before services are rendered reduces the risk of claim denials. We check for active coverage, benefits, and any pre-authorization requirements. This verification process ensures that the services provided are covered, preventing billing issues down the line. Our team contacts insurance companies to verify details and confirm eligibility, reducing the likelihood of denied claims due to coverage issues.
Pre-Authorization Management: Certain treatments and procedures require pre-authorization from insurance companies. We handle this process efficiently, obtaining necessary approvals in advance. This proactive approach minimizes delays and ensures that claims are processed smoothly. Pre-authorization management involves coordinating with insurance companies, submitting required documentation, and following up to secure approvals.
Coding Accuracy Audits: Accurate coding is essential for maximizing reimbursements. We conduct regular coding audits to ensure that all services are coded correctly and in compliance with payer requirements. These audits help identify and correct coding errors, reducing the risk of claim denials. Our coding experts review medical records and ensure that the appropriate codes are used for the services provided, adhering to the latest coding guidelines and standards.
Claims Submission and Follow-Up: Timely submission of claims is crucial for maintaining cash flow. We submit claims promptly and follow up on unpaid claims to ensure timely reimbursements. Our team actively monitors the status of submitted claims and takes immediate action on any issues that arise. We communicate with payers to resolve discrepancies, address denials, and expedite payments.
Patient Statements and Billing Inquiries: Clear communication with patients is essential for prompt payments. We generate and send detailed patient statements, keeping patients informed about their outstanding balances. Additionally, we handle billing inquiries from patients, providing them with the information they need to make timely payments. Our customer service team is available to answer questions and address concerns, ensuring that patients understand their financial responsibilities.
Payment Posting and Reconciliation: Accurate payment posting and reconciliation are critical for maintaining consistent financial records. Our team accurately posts payments received from insurance companies and patients, and reconciles accounts to ensure consistency. This process helps identify any discrepancies and ensures that your financial records are up-to-date. We match payments to the corresponding claims, track adjustments, and verify that all transactions are recorded accurately.
Denial Management and Appeals: Denied claims can significantly impact your practice’s revenue. Our team manages denied claims and handles the appeals process, ensuring that denied claims are re-submitted with the necessary corrections and supporting documentation. We work diligently to resolve denials and maximize reimbursements. Our denial management process involves analyzing denial reasons, correcting errors, and providing additional information to support appeals.
Reporting and Analytics: Comprehensive reporting and analytics provide valuable insights into your billing performance. We provide detailed reports on submitted claims, payment statuses, denial rates, and cash flow trends. These reports help you make informed decisions and identify areas for improvement. Our analytics tools track key performance indicators (KPIs) and provide actionable insights to enhance your billing processes.
AR Follow Up
Take control of your financial future with our specialized accounting services – Click here for details.
Audit Support
Let us handle the numbers, so you can focus on growth – Contact us now for accounting services.
Social Media Marketing
Elevate Your Brand's Voice – Social Media Marketing That Connects, Engages, and Grows!
Website Development
Transform Your Vision into Reality – Stunning, Functional Websites Built for Success!
Statistics and Impact
Studies show that efficient medical billing and accurate charge creation can lead to a 20-30% increase in revenue for medical practices. Additionally, practices that implement optimized billing processes see a 25% reduction in claim denials and a significant improvement in cash flow. Effective problem list management and comprehensive billing services further enhance coding accuracy and patient care. These enhancements not only boost your financial health but also enhance the efficiency of your practice.
Effective problem list management also contributes to the overall quality of care provided to patients. By maintaining accurate and up-to-date problem lists, healthcare providers can ensure that all relevant diagnoses are considered during patient care, leading to better treatment outcomes.
Our comprehensive approach to medical billing and charge creation ensures that every aspect of the billing process is handled with precision and care. From verifying patient insurance coverage to managing denied claims, we cover all bases to ensure that your practice receives the revenue it deserves.
Meet Our Doctors
Dr. Faika Khan
Dr. John Muney
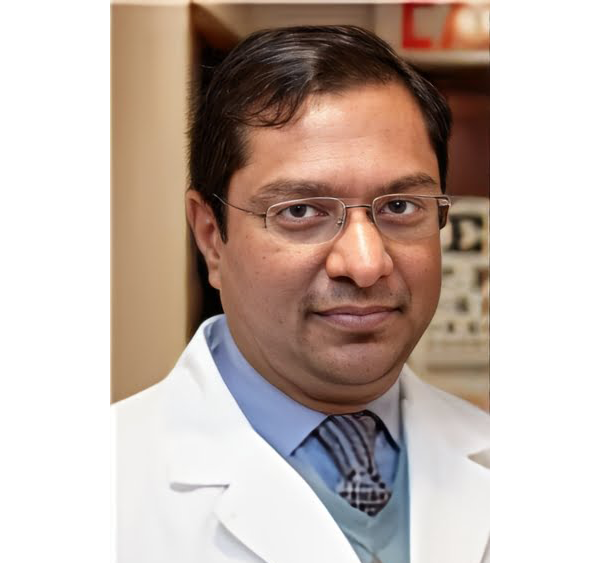
Dr. Ravindra Kashyap
Dr. Valerie Brutus
Your questions answered
Frequently Asked Questions (FAQs)
What is Medical Billing & Charge Creation?
Medical Billing & Charge Creation involves the accurate entry of charges based on services provided and the submission of claims to payers. It ensures timely reimbursements and compliance with regulatory standards.
How can accurate charge creation improve our practice's revenue?
Accurate charge creation minimizes billing errors, ensuring that all services provided are billed correctly. This leads to optimized revenue and reduces the risk of claim denials.
How do you ensure compliance with payer guidelines?
Our team stays up-to-date with the latest payer guidelines and regulatory standards. We ensure that all billing practices align with these requirements, minimizing the risk of penalties and fines.
What kind of reporting can we expect from your Medical Billing services?
We provide detailed billing reports, including information on submitted claims, payment statuses, and any outstanding balances. These reports give you clear insights into the financial health and performance of your practice.
How do your services help reduce claim denials?
By ensuring accurate charge creation and timely billing submission, we minimize the risk of claim denials. Our proactive approach to billing helps ensure that claims are processed correctly and promptly.
What is the importance of managing problem lists in medical billing?
Managing problem lists ensures accurate and comprehensive patient documentation. It helps in precise coding, reducing billing errors, and improving patient care coordination.
What are the benefits of outsourcing Medical Billing & Charge Creation to Health Care Protectors?
Outsourcing these services to us ensures accurate and efficient billing processes, compliance with regulatory standards, personalized support, and detailed financial reporting. This allows you to focus on patient care and strategic decision-making.
How do we get started with Health Care Protectors' Medical Billing & Charge Creation services?
Getting started is simple. Just contact us through our website or give us a call. Our team will guide you through the process and customize a billing plan that meets your practice’s needs.
Ready to optimize your revenue cycle and improve cash flow? Contact Health Care Protectors today to learn more about our expert Medical Billing & Charge Creation services, including effective problem list management, and how we can help your practice thrive.