🏥 Grow Revenue & Improve Care With CCM & RPM

Grow Revenue & Improve Care With CCM & RPM
CCM and RPM programs offer guaranteed per-patient CMS reimbursements with no
added staffing or operational burden. The service includes full support for enrollment,
portal, care plan, monthly monitoring, billing and 24/7 assistance — while allowing
providers to maintain complete control over patient relationships and care strategies.
✅ What We Do
We help practices like ABC Clinic unlock Medicare-covered revenue through fully managed Chronic Care Management (CCM) and Remote Patient Monitoring (RPM) — all HIPAA-secure and 100% compliant.
✔️ No staffing needed — we handle everything: patient outreach, scheduling, enrollment, monitoring, billing, and compliance.
✔️ Stay in control — you maintain full oversight of patient relationships and care plans.
✔️ Proven ROI — our clinics earn $150K–$200K+ annually in new Medicare reimbursements.

📋 Chronic Care Management (CCM) Plans
| Time/Patient | CPT Code(s) | Average Reimbursement | Basic Service (No Portal) | With Portal & Dashboard | Full-Service |
|---|---|---|---|---|---|
| 20 mins | 99490 | ~$62 | $10 | $15 | $25 |
| 40 mins | 99490 + 99439 | ~$109 | $20 | $25 | $35 |
| 60 mins | 99490 + 2×99439 | ~$158 | $25 | $30 | $40 |
📋 For Complex CCM
| Time/Patient | CPT Code(s) | Average Reimbursement | Basic Service (No Portal) | With Portal & Dashboard | Full-Service |
|---|---|---|---|---|---|
| 60 mins | 99487 | ~$132 | $25 | $30 | $40 |
| 90 mins | 99487 + 99489 | ~$200 | $45 | $50 | $60 |
📋 Remote Patient Monitoring (RPM) Plans
| Service Tier | CPT Code(s) | Average Reimbursement | Setup Only | Monitoring Only | Full-Service |
|---|---|---|---|---|---|
| One-Time Setup | 99453 | ~$19 (one-time) | $0–$10 | N/A | N/A |
| Monthly Monitoring | 99454 + 99457 | ~$105 | N/A | $15 | $25 |
| Extended Monitoring | 99458 | ~$40 (each add’l 20 min) | N/A | +$10 each add’l 20 min | +$10 each add’l 20 min |
📌 How CCM & RPM Works
1️⃣ Identify & Enroll
We help you identify eligible Medicare patients (2+ chronic conditions or high-risk profiles). If needed, we coordinate an Annual Wellness Visit (AWV) to kickstart the program.
2️⃣ Outreach & Consent
Our care team explains the program to patients, obtains consent, and logs all documentation in a HIPAA-compliant portal.
3️⃣ Care Plans & Devices
We build personalized care plans for CCM and handle FDA-approved device shipping for RPM (BP cuffs, glucometers, etc.). Patients and providers can view care plans and readings in real time.
4️⃣ Monthly Monitoring
CCM: Clinical staff deliver 20–60+ minutes/month of non-face-to-face support (calls, care coordination, medication reminders).
RPM: Devices auto-sync vitals daily, with real-time alerts for abnormal readings. Our team flags any issues for follow-up.
5️⃣ Billing & Compliance
Everything is tracked: time logs, notes, actions — all audit-ready. You get a monthly summary to bill Medicare or we can handle submission for you.
6️⃣ Ongoing Support
Patients have access to their portal dashboard, and you receive performance dashboards, risk reports, and regular reviews to optimize care and maximize revenue.
💵 Simple, Transparent Pricing
| Service | Monthly Cost (per patient) | Includes |
|---|---|---|
| CCM | $10–$60 | Enrollment, portal, care plan creation, monthly monitoring, compliance, billing |
| RPM | $10–$35 | FDA-approved device, shipping, daily monitoring, real-time alerts, patient & provider portal, billing |
✅ No upfront fees. No minimum volume. Pay only for the services you use.
✅ Most practices generate $150K–$200K+ each year with recurring Medicare reimbursements.
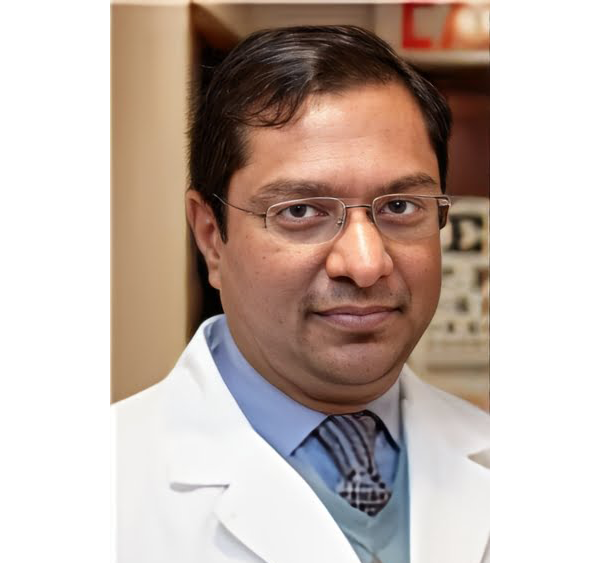
Meet Our Doctors
Dr. Faika Khan
Dr. John Muney
Dr. Ravindra Kashyap
Dr. Valerie Brutus
Your questions answered
Frequently Asked Questions (FAQs)
How much can our practice really earn?
On average, our clients see $150K–$200K+ annually in new, recurring revenue — fully backed by Medicare reimbursements.
Is this HIPAA-compliant?
Yes. All data, monitoring, and communications run through our secure, HIPAA-compliant portal.
Who does the work?
We do! Our team manages patient outreach, enrollment, monitoring, alerts, reporting, and billing documentation. Your staff stays focused on in-person care.
What if we don’t have extra staff?
You don’t need any — our system is fully managed. No new hires, no additional admin load.
How is the billing handled?
All care time and device readings are tracked in the portal. You get a ready-to-submit monthly billing report — or we can submit claims on your behalf.
Is this really risk-free?
Yes — there’s no upfront cost and you only pay per patient per month. If you’re not satisfied, we’ll work with you to make it right — you stay in full control.
✨ Grow Your Revenue, Not Your Workload
Ready to explore? Let’s set up a quick, no-pressure call to walk through your numbers.