Medical Billing Audit
Ensure Accuracy and Compliance with Our Expert Medical Billing Audit Services!

Comprehensive Medical Billing Audit
At Health Care Protectors, we offer specialized Medical Billing Audit services designed to enhance the accuracy and compliance of your billing processes. Our team is dedicated to identifying and resolving discrepancies, ensuring your practice operates efficiently and maximizes revenue. With our comprehensive audit services, you can confidently navigate the complexities of medical billing and focus on delivering exceptional patient care.
Why Medical Billing Audits Matter
Medical billing audits play a critical role in maintaining the financial health of your practice. Regular audits help identify errors, reduce claim denials, and ensure compliance with ever-evolving regulations. Here’s why you should consider our Medical Billing Audit services:
- Accuracy and Compliance: Audits help detect and correct billing errors, ensuring your practice remains compliant with payer guidelines and regulatory requirements.
- Revenue Optimization: By identifying underpayments and missed charges, audits help maximize your practice’s revenue.
- Risk Mitigation: Regular audits minimize the risk of penalties and fines by ensuring adherence to billing standards and reducing the likelihood of fraudulent claims.
Why Choose Healthcare Protectors
Our Approach
At Health Care Protectors, we adopt a meticulous and data-driven approach to medical billing audits:
- Thorough Review: We conduct a comprehensive review of your billing records, examining every detail to identify discrepancies and errors.
- Root Cause Analysis: Our team investigates the underlying causes of billing issues, providing targeted solutions to prevent future occurrences.
- Compliance Checks: We ensure your billing practices align with current payer guidelines and regulatory standards.
- Detailed Reporting: We provide clear and actionable audit reports, highlighting areas for improvement and offering recommendations to optimize your billing processes.
- Free Initial Audit: To help you understand where your practice stands, we offer a free initial audit to assess your strengths and improvement areas.
Statistics and Impact
Studies show that medical practices can experience a 10-20% increase in revenue by conducting regular billing audits. Additionally, practices that implement audit recommendations see a 30% reduction in claim denials and a significant decrease in billing errors. These improvements not only boost your financial health but also enhance the efficiency of your practice.

AR Follow Up
Take control of your financial future with our specialized accounting services – Click here for details.
Audit Support
Let us handle the numbers, so you can focus on growth – Contact us now for accounting services.
Social Media Marketing
Elevate Your Brand's Voice – Social Media Marketing That Connects, Engages, and Grows!
Website Development
Transform Your Vision into Reality – Stunning, Functional Websites Built for Success!
Our Denial Management Process
- Identification: We proactively identify claims rejected due to clerical deficiencies or denied by insurance companies. Timely action is critical.
- Investigation: Our team investigates the root causes of denials. Was it a coding issue? Did documentation fall short? We leave no stone unturned.
- Resolution: Once identified, we address denials promptly. Whether it’s resubmitting claims, appealing decisions, or providing additional documentation, we take action.
- Prevention: Prevention is key. We analyze patterns, implement corrective measures, and educate your team to minimize future denials.
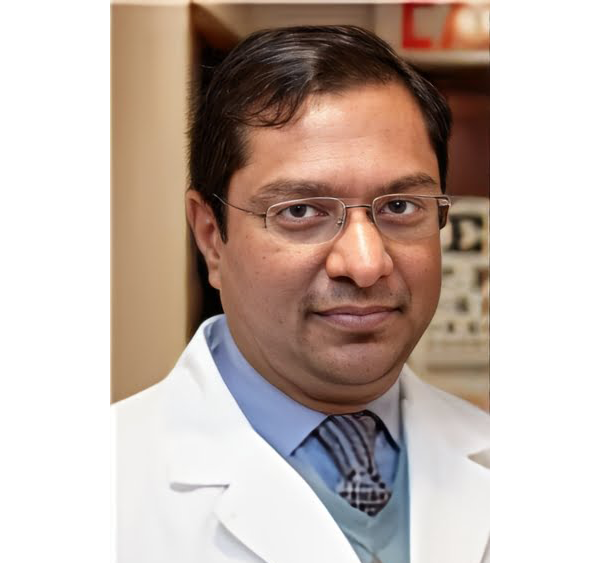
Meet Our Doctors
Dr. Faika Khan
Dr. John Muney
Dr. Ravindra Kashyap
Dr. Valerie Brutus
Your questions answered
Frequently Asked Questions (FAQs)
What is a Medical Billing Audit?
A Medical Billing Audit is a thorough examination of your billing records to identify errors, ensure compliance with regulatory standards, and optimize revenue. It involves reviewing claims, payments, and coding practices to detect discrepancies and improve accuracy.
How often should we conduct a Medical Billing Audit?
It is recommended to conduct a Medical Billing Audit at least annually. However, more frequent audits may be necessary for practices with high claim volumes or those undergoing significant changes in billing processes.
What are the common issues identified in a Medical Billing Audit?
Common issues include incorrect coding, missing or incomplete documentation, underpayments, overpayments, and non-compliance with payer guidelines. Our audits help identify and address these issues to ensure accurate and compliant billing practices.
How can Medical Billing Audits improve our practice's revenue?
By identifying billing errors and missed charges, audits help optimize your revenue. They also reduce claim denials, ensuring timely and accurate payments. Implementing audit recommendations can lead to significant financial improvements for your practice.
What kind of reporting can we expect from your Medical Billing Audit services?
We provide detailed and actionable audit reports, highlighting areas for improvement and offering recommendations to enhance your billing processes. These reports give you clear insights into the accuracy and compliance of your billing practices.
How do your audits help reduce the risk of penalties and fines?
Our audits ensure compliance with payer guidelines and regulatory standards, minimizing the risk of penalties and fines associated with billing errors and fraudulent claims. By adhering to best practices, your practice can operate with greater confidence and security.
How do we get started with Health Care Protectors' Medical Billing Audit services?
Getting started is simple. Just contact us through our website or give us a call. Our team will guide you through the process and customize an audit plan that meets your practice’s needs.
Ready to ensure accuracy and compliance in your billing processes? Contact Health Care Protectors today to schedule your free initial audit and discover your practice’s strengths and improvement areas.